Practical Acupuncture for Bloat
C.A. Krowzack, DVM
Introduction
I received my Doctor of Veterinary Medicine from the University of Illinois Champaign/Urbana in 1977. In 1999 I completed the American Veterinary Acupuncture Society course on acupuncture. I was in private practice until 2004 and utilized acupuncture and herbal therapies in addition to traditional Western medicine in my practice. After practice I taught veterinary technology at The Vet Tech Institute of Fox College in Tinley Park, Illinois and included a module on alternative medicine in my Pharmacology course.
What is Acupuncture?
Many people consider acupuncture to be a form of voodoo. In Traditional Chinese Medicine (TCM) acupuncture points (acupoints) are locations of focused energy along channels (meridians) of energy. In TCM illness and disease are manifestations of imbalances or blockages of energy in the body and acupuncture balances or releases the energy blockage.
In Western Medicine anatomical and neurophysiological research has shown acupoints to be either at the end point of nerve fibers or where nerve fibers penetrate the body’s tissue planes. Stimulation of acupoints releases detectable neurochemicals and hormones which can have effects throughout the body.
Because of the patterns of embryological and neuroanatomic development, acupoints may be quite removed from the organ system they effect. The Stomach Meridian, for example, starts on the face, runs along the underside of the body, up and over the flank and onto the lateral (outside) aspect of the hind leg, ending on the toe.
Another characteristic of acupuncture that confuses people is the points on meridians which seem unrelated can affect other organ systems. For example, the Bladder Meridian contains points for many systems besides the urinary tract.
With that in mind, I will describe several acupoints that you, as an owner, can find and use with acupressure and may help to save your dog’s life.
What is Bloat?
Commonly called bloat, the medical term is gastric dilation/volvulus or GDV.
Gastric dilation is a large accumulation of gas in the stomach and can occur with or without twisting of the stomach, volvulus. Both are emergency situations, but volvulus is a complicating factor which significantly decreases the likelihood of a good outcome. Some breeds, including deep chested and giant breeds, have a high incidence of bloat. For example, in Great Danes up to 42%1 of the dogs may be affected. But I’ve seen bloat in a spaniel and even a cat. Both the Irish wolfhound and Scottish deerhound can be affected.
Because it is such a devastating illness much research has been done over many years. Unfortunately, no definitive answers are currently available. Genetics would seem to play a role given the high percentage of incidence in certain breeds and DNA research is being conducted . Diet, exercise, and temperament have all been implicated at one point. So, what do we know? Nutrition studies point to dry kibble and once a day feeding. Feeding from elevated bowls or on the floor doesn’t affect the incidence. Adding other foods to dry kibble seems to decrease the incidence although there is no consensus on what other foods. Adding canned food, or eggs, or table food, or raw foods all seem to have the same beneficial effect. High strung dogs seem to have a greater likelihood of developing bloat, but it is uncertain just how much of an effect it has.2 What about exercise? For a long time, the rule of thumb was not to let your dog exercise after eating—which sounds suspiciously like no swimming after a meal, an idea which has been debunked. Studies haven’t borne that out.
So, what do we do for prevention? Raw food advocates will say feed raw. Dry food advocates want the ease and guaranteed nutrition. If an owner wants to play it safe, if they are feeding dry kibble they should add something to the food, preferably a balanced AAFCO certified canned food or AAFCO certified raw food to avoid unbalancing the nutrients in the diet. Feeding twice a day makes sense since it decreases the amount of material in the stomach at any given time. Preventative stomach tacking (suturing the stomach in position) could be considered and is recommended in Great Danes. That can be done at the time of a spay or neuter. There are veterinarians who can perform a stomach tack with a laparoscope.
Signs of Bloat
Dogs experiencing bloat may show signs of restlessness, pacing, reluctance to lie down and attempts to vomit. They will retch but nothing with come up. The sound is something like: ga-a-ack. They gulp and lick their lips. As it progresses the owner will notice the dog looking fuller in the abdomen or rib cage. Pressing on the abdomen will cause discomfort or pain. If you thump with a finger behind the ribs on the left side the abdomen will sound like a drum. As it progresses, the dog’s gums will start to pale, then turn gray to bluish, their heart rate will increase indicating shock and they will get weaker, eventually collapsing. The stagnant blood absorbs toxins from the deteriorating stomach and in a worsening cascade of events the dog goes into endotoxemic shock (like toxic shock syndrome). Once a dog reaches this point, they are unlikely to survive. Remember: this is an emergency! Don’t wait to see a veterinarian! It is better to be wrong than to have your dog die.
What to Do
First, if you think even possibly that your dog is bloating, call your vet immediately! Think of this as calling 911 if your house is on fire. Can you try to fight the fire? Yes. Should you? No.
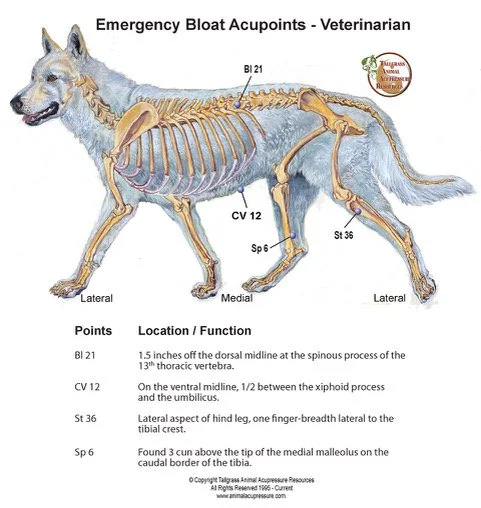
But there are useful acupuncture/acupressure points which can buy you time while you get to the veterinarian. Disclaimer: these points will not help if volvulus has already taken place, so it’s better to start at the first signs of bloat. The main “bloat point” is Stomach 36 (ST 36). It is on the lateral (outside) aspect of the hind leg, below the stifle (knee) in the body of the Tibialis anterialis muscle. In some individual, especially greyhounds, this muscle may be very well developed. To find ST36 put your hand on the dog’s leg at the front of the hock (heel) joint and find the tibia, or shin bone. Follow the tibia up the leg. It becomes a sharp ridge. Just below the stifle you will feel a bony prominence. This is the tibial crest. Let your hand slide over the ridge onto the lateral aspect of the leg. If you feel very gently with your fingertip, you may feel a slight indentation--ST36. Another way to find ST36 is to bend the dog’s leg slightly. Starting at the patella (kneecap) slide your hand down the stifle. The first prominence after the patella is the tibial tuberosity. The second ridge down is the tibial crest. Don’t be discouraged if you can’t feel ST36 specifically. If you are in the right area and if you massage vigorously or press firmly, you can still stimulate the energy release. If your dog is having a stomach or spleen problem this point will be sore and he may jerk his leg away.
The second acupoint to monitor is Bladder 21 (BL 21). The Bladder Meridian runs down the back on both sides of the spine. First, measure the 10th rib width compared to your finger. This is a unit of measurement called a cun (“soon”). Next, feel the end of the 13th rib (the last rib) and follow it up to the attachment at the spine. Find the vertebrae behind it. BL 21 is a depression halfway between these two vertebra (T13 and L1) 1.5 rib widths (cun) lateral to the midline. Please note that the size of a cun is relative to the size of the dog which is why you measure the rib.
BL 21 is a diagnostic point for the stomach. If a dog has a stomach disorder this point will be painful. Their skin may ripple when you press the point, or the muscles spasm, or the dog may drop their back because it is painful to touch there.
The final point is Conception Vessel 12 (CV12). The CV Meridian runs down the ventral midline of the body. CV12 is a depression halfway between the umbilicus (navel; belly button) and the end of the sternum. CV 12 is the “alarm point” for the stomach. Pressing here will make the dog groan, grunt in pain or whimper. See illustration.
Putting It to Work
You have the information; now how do you use it? It is late at night. Your dog wakes you. He is restless and anxious. He tries to gag or vomit but nothing comes out. You feel his sides but you aren’t sure if he is fuller or if his abdomen is hard (or maybe you are). Find ST36 and press. He jerks his leg away. Find CV12 and press up. He whines. Find BL21 and press. He flinches. CALL YOUR VETERINARIAN IMMEDIATELY!!! Knowledge and use of the acupuncture or acupressure points is not a substitute for emergency veterinary care. If possible, while one person is phoning, the other person should vigorously massage ST36. Even dig a fingernail into the point. It may take ten to fifteen minutes to get a response but it will work IF volvulus (twisting of the stomach) is not present. The dog will start to belch or pass gas when you are successful. Don’t quit, though. If possible, have someone continue to massage ST36 (adding CV12 helps) during the trip to the emergency clinic or your veterinary clinic. Massaging for 20 minutes is a typical treatment period.
Once at the emergency clinic your dog may still need to have his stomach pumped of residual fluid, gas, and food. Intravenous fluids and monitoring for signs of toxemia may be necessary. Some of the toxic side effects of bloat (cardiac arrythmias, stomach wall necrosis) may not appear for twenty-four to forty-eight hours, so intensive care monitoring may be necessary. Acupressure treatment can help you win the battle, but the war isn’t won until the danger period is past.
Editor’s note: the author retains all copyright privileges for this article.
1. Great Dane Update, A Nestle Purina Publication Dedicated to Great Dane Enthusiasts Vol. 15, Summer 2017
2. The Purdue Bloat Study
Bloat Notes: News From the Canine Gastric Dilatation-Volvulus Research Program
School of Veterinary Medicine
Purdue University
Illustration reprinted with permission from Tallgrass Animal Acupressure Resources
Spotlight on Health - Midwest Wolfhound - Summer edition 2019
Calcinosis Circumscripta
Article by Risha Cupit-Berzins & Dave Berzins
What is calcinosis circumscripta?
Calcium deposits in soft tissue
Where do they occur?
Often in subcutaneous tissue of the hind feet, but they can occur in other areas of the limbs as well as the tongue, lips, and other soft tissues.
Other facts:
Most often they are a single mass, but they can be in multiple locations.
They are often 0.5-3 cm in diameter.
They have a chalky, white appearance when opened up.
Reference:
Tafti AK, Hanna P, Bourque AC. Calcinosis circumscripta in the dog: a retrospective pathological study. J Vet Med A Physiol Pathol Clin Med. 2005 Feb;52(1):13-7.
How to become an expert in bandaging an Irish Wolfhound’s foot
Since he was 1-2 years old, Hubig had a small growth on his right back foot near the large foot pad that we knew was a calcinosis circumscripta. Through a non-related hound of ours from Ireland (Lilagh) and Hubig’s aunt (Ursuline), we had experience with them in the past, both on hind feet. Lilagh’s was surgically removed without much issue, but that was not the case with Ursuline. Her calcinosis was removed when she was 11 months old and she had issues with the surgical site as it never fully healed and would occasionally become infected through her remaining years (she lived to 10.5). Because of the issues with Ursuline, we opted to not remove Hubig’s calcinosis because it was not hindering or bothering him.
Hubig with his foot wrapped
However, in early May 2018, when Hubig was 5.5 years old, everything changed as his calcinosis circumscripta was getting larger and had gotten to the point that the skin was very thin. On a walk one Friday, the skin thinned enough that it no longer protected his foot and within a day, there was a raging infection and was oozing a mostly chalky liquid with a tinge of blood. Our floor had milky/chalk streaks all over. We messaged one of our veterinarians, who texted back it should be removed ASAP. The next Monday (May 14), he went in for surgery. Our vet removed the growth and the skin was beautifully sutured together. She put him on 10 days of Cephalexin and we changed the bandage as directed, and his foot looked like it was healing nicely. Each time he went outside, we double-bagged his foot and only kept him in the yard. But then a couple of days beyond day 10, his foot was painful and when we removed the bandage, it was obviously infected; the skin around the incision was inflamed, red, wet, and the sutures had split apart. Our vet put him back on Cephalexin until a culture came back (and eventually placed on Cipro) and rewrapped his foot after removing the non-functioning sutures. He now had a wound that was around 2.5 inches in diameter.
Though it was thought the wound would heal within weeks, the reality became that treating his foot wound would become part of our lives for the next 16 months. The wound was in a terrible spot for healing, being close to the ground and in an area that would flex with walking. His foot was nearly healed a few times during the 16 months, only to have something that caused it to become infected again. As before, his bandaged foot was wrapped in bags to keep it clean when he was let outside into the yard. Despite this, reinfections would expand the wound back to the starting point. He also developed proud flesh that limited healing. Overall, it was incredibly frustrating for both humans and Hubig.
Hubig’s foot healed
For many months, we worked with our veterinarians and a veterinary wound care specialist to come up with the best way to address it. Under veterinary supervision, we used many different products and medications. Some worked, but often it seemed they tended to only do so for a given amount of time. Others were not appreciably effective. Throughout treatment time, bandage changes seemed to be most effective if done every 36-48 hours. Changing the bandage more frequently often did not allow enough time for healing, as the process of removing the bandage sometimes undid any progress, whereas allowing the bandage to be on for longer periods kept the oozing area too wet.
Over time, we did dry, wet, and wet-to-dry bandages. Various vet wrap, gauze, telfa pads, cast wrapping, and other bandages were used. Collagen products were tried, such as collagen gels/sprays (Collasate) and a few collagen scaffolds. The scaffold made from porcine collagen provided a setback, however, as we found out he was allergic to it but one scaffold from bovine collagen worked well for a time. Also tried were a colloidal silver cream, drying powder, antibiotic ointment (Fura-zone), antibiotic sprays, antifungals (TrizUltra), a steroid/antibiotic combination spray (GentaSpray), Manuka honey patches, and raw Manuka honey.
After wrapping his foot at least 250 times, we have our system in place and Hubig does too. We tell him “get in place” and he climbs up on the ottoman, and often falls asleep, snoring, while we wrap his foot. Since January, we have used the same procedure and while it has taken many months to heal, we generally did not have a setback during this time. I use a gauze pad with a cleanser/antifungal (TrizUltra) to clean the wound/area and then slightly dry. Next, about 3-5 sprays of the GentaSpray is applied to the wound with any excess dried with a gauze pad. I put 1 gauze pad in between the pads of his foot to absorb any dampness and to keep from getting a fungal infection. On a telfa pad, I apply a pea-sized dollop of Collasate on it, place it on the wound and then apply 3-4 gauze pads and wrap cast padding around his whole foot about 10 times. Next, vet wrap is wrapped in the opposite direction that the cast padding was done at least 10 times, checking that it is not too tight. Finally, a small piece of Elastikon tape is applied over the end of the vet wrap to keep it from coming loose. After we are done, we tell Hubig he is a good boy and that we are done, and he gets on the sofa and gives Dave kisses.
Post Surgery Photo
Hubig is normally a very active dog, taking part in agility, obedience, rally, and scent work. In this time, he was the very best boy anyone could dream of having. He always left that bandage alone, which was absolutely remarkable. On a couple of occasions, maybe out of boredom, he licked the bandage, but a quick “No. Leave it!” would be enough to redirect his attention, to something that was allowed. He got extra love, ear scratches, and took my place next to Dave at night, watching TV. In all these many months, we trained him in the house, working on scent work and some obedience to preoccupy his mind.
Normally in summer Hubig gets to have dinner with us outside at a favorite local restaurant, and go for Babe’s vanilla ice cream with peanut butter drizzle, afterward, but he’s been restricted from those things as well, so we don’t potentially introduce new pathogens. We have taken him to Babe’s and brought his ice cream treat to the van for him, though. We should be able to let him take a real trip to do both, soon. He certainly deserves the world for being so good through all of this.
GLIWA Board Report 5-21-16 Rescue
mIDWEST wOLFHOUND - sPRING 2016 eDITION
By Robert and Debbie Greene
FINN
It has been a couple of busy months! We were contacted by an owner in Naperville about her 10 month old wolfhound Finn. When she purchased Finn she took him to the vet to find that he had virtually every worm / parasite possible. He was treated for that then got Giardia. Finn had OCD and had surgery to correct it.
We have a 31 page medical file from the vet! $11,000 later…….. The owners / vet said he has IBS and was on a special diet. They were very afraid he would get sick again so they made sure he never touched dirt/grass/twigs to his mouth. They saw him eat grass when we were there and pulled it out of his mouth. He had no fenced in place to run as they lived on a golf course and a fence would obstruct the view. He had only been walked on a leash on the sidewalk so he wouldn’t get into anything dirty.
Fin
He has no AKC Papers and hasn’t given us a breeder name. She said they didn’t file the papers. The owners said they needed to re-home him because he had become very aggressive. Biting them and chasing them through the house. They slept with him in their kitchen at night. We met with them at their house and it took three more weeks to get him to our house. Finn He is fitting in well. He is a complete puppy and has had no training except sit, shake and down. He was VERY toy aggressive when he got here and that is in the vet report also. He was banned from playing with other dogs and staff because he wouldn’t play nice. I have gotten him to a point I can now transfer a treat or a stick for an object he is NOT supposed to have. Very confusing for him because baby toys and dog toys look alike to babies and dogs! 95% of the time he is a very sweet dog and a big baby. We are thinking at this point that we will keep him here if things work out.